Rose City Physical Therapy specializes in orthopedic and sports injury physical therapy. Please visit our staff page to learn more about our Board-Certified Orthopedic Specialists. Our highly-trained physical therapists have decades of experience in orthopedic physical therapy and will work with you to design individualized treatment programs to help reduce your pain, regain normal movement, and get back to your regular activities. Contact us to schedule an appointment today!
Article Featured on MoveFowardPT, Reviewed by Karl Kolbeck, PT
As many as 40% of people will experience sciatica during their lifetime, according to Harvard Medical School, and the condition becomes more frequent as one ages. Although sciatica is among the more common causes of pain, it is also often incorrectly categorized and misunderstood.
What is sciatica? What are its common triggers? What are the signs and symptoms? How is it diagnosed? Can it be prevented? How is it best addressed and treated?
Lumbar radiculopathy (also known as sciatica or radiculitis) is a condition that occurs when a nerve in your low back is injured, pinched, or compressed, causing pain or other symptoms that can extend from the low back to the hip, leg, or foot. Sciatica can be caused by sudden trauma or by long-term stress affecting structures in the back. It most often affects people aged 30 to 50 years.
How Does it Feel?
Sciatica can cause pain, muscle tightness and weakness, or other symptoms. The pain usually starts in your lower back, and can travel to your hip, leg, or foot. The location of the pain can vary depending on which nerve in your back is affected and how much it is irritated. Greater irritation causes the pain to spread farther. Spreading pain usually affects one leg, but may affect both legs. Pain and other symptoms can be constant or come and go, and your pain may vary in intensity.
If a nerve or nerve root (the nerve branches deep in your back at the spine level) is severely pinched or compressed it can cause severe pain, muscle weakness, or extreme movement problems. Surgery may be recommended in more severe cases. On rare occasions, nerve compression can cause bladder control or bowel function problems, in which case immediate surgery is recommended.
Rose City Physical Therapy can determine the details of your condition and discuss what a successful treatment plan consist of, and whether consultation with a surgeon is necessary. Our physical therapists will work with your physician or surgeon to determine your best treatment.
Signs and Symptoms
Sciatica can cause a variety of symptoms and signs. The type and location of your symptoms will depend on the amount of pressure being placed on the affected nerve(s). Symptoms and signs may include:
- Pain and/or pressure in the back, hip, leg, and/or foot/feet
- Pain that can be throbbing, aching, shooting, sharp, dull, or burning
- Limitation in or inability to bend or rotate the back
- Numbness or tingling in the back, hip, leg, or feet
- Leg weakness
- Increased pain when coughing, sneezing, reaching, or sitting
- Inability to stand up straight; being “stuck” in a position such as stooped forward
- Pain with sitting and difficulty getting up from a chair
- Inability to remain in one position for a long period of time, such as sitting or standing, due to pain
- Pain that is worse in the morning
- Limping when walking
The pain or other symptoms can occur in one or both limbs. Your pain may present in different locations at different times, and can change depending on your activity or body positioning. For example, pain can lessen or worsen when walking versus sitting, or lying down versus standing up.
How Is It Diagnosed?
Rose City Physical Therapy will conduct a thorough evaluation including a review of your health history. Your therapist will ask you detailed questions about your injury, such as:
- Do you have loss of control of your bladder or bowel? CAUTION: Contact a medical professional immediately if you experience this condition.
- How and when did the pain start?
- At what time of day is it worse?
- What type of discomfort do you feel, and where do you feel it?
- What are you unable to do right now in your daily life due to the pain?
Your physical therapist will perform a variety of tests to identify potential complications and assess the severity of your symptoms. These tests are designed to check for symptoms and clinical signs including:
- Difficulty moving
- Muscle weakness or tightness
- Changes in skin sensation (numbness)
- Changes in reflexes
- Joint stiffness
- Changes in posture
- Difficulty walking or balancing
If your physical therapist finds any of the above problems, physical therapy treatment may begin right away. Our goal at Rose City Physical Therapy is to help get you on the road to recovery and back to your normal activities as quickly and safely as possible.
If testing indicates any concerns, your physical therapist will consult your physician or surgeon regarding the need for special diagnostic testing, such as magnetic resonance imaging (MRI).
Our board-certified physical therapists at Rose City Physical Therapy will work closely with your physicians and other health care providers to ensure you receive an accurate diagnosis, treatment, and the care you need.
How Can a Physical Therapist Help?
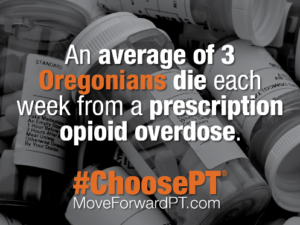
In all but the most extreme cases of sciatica, conservative care (such as physical therapy) often produces better, faster, and more cost effective results than surgery or pain medication (such as opioid medication).
Your physical therapist will work with you to design a specific treatment program that will speed up your recovery, including exercises and treatments that you can do at home. Physical therapy will help you return to your normal lifestyle and activities. The time it takes to heal your condition may vary, but improvement can be achieved in 4 to 8 weeks when a proper posture, pain reduction, stretching, and strengthening program is implemented.
During the first 24 to 48 hours following your diagnosis of sciatica, your physical therapist may advise you to:
- Protect the area by avoiding activity that causes worsening symptoms, such as heavy lifting, sitting, bending and twisting, or standing.
- Avoid too much bed rest.
- Stay active around the house, and go on short walks several times per day. Movement will decrease your pain and stiffness, and help you feel better.
- Apply ice packs to the affected area for 15 to 20 minutes every 2 hours.
- Sit in supportive, firm chairs. Prolonged resting in soft couches or easy chairs may make your pain worse.
- Consult with a physician for further services, such as medication or diagnostic tests.
Your physical therapist will educate you about specific exercises designed for patients with sciatica. For example, water exercises can be a great way to stay physically active when other forms of exercise are painful. It’s important to note that some traditional exercises, such as those that involve twisting, bending, or weight lifting may aggravate your sciatica if not conducted with the proper form. We will design an individualized exercise program to reduce your leg pain and meet your specific needs.
Rose City Physical Therapy will work with you to:
Reduce pain and other symptoms. We will help you understand how to avoid or modify the activities that caused the injury, so healing can begin. Your therapist may use different types of treatments and technologies to control and reduce your symptoms. Your treatment, based on your condition, may include specific motion exercises, mechanical
traction, and electrotherapy such as Interferential Current or Transcutaneous Electrical Nerve Stimulation (TENS).
Improve motion. We will choose specific activities and treatments to help restore normal movement. These might begin with “passive” motions that your physical therapist performs for you to move your spine, and progress to active exercises and stretches that you do yourself. You can perform these motions at home and in your workplace to help hasten healing and pain relief.
Improve flexibility. We will determine if any of the involved muscles are tight, start helping you to stretch them, and teach you how to stretch them at home.
Improve strength. If your physical therapist finds any weak or injured muscles, they will teach you the correct exercises to steadily restore your strength and agility. “Core strengthening” exercises are commonly used to restore the strength and coordination of muscles around your back, hips, abdomen, and pelvis.
Improve endurance. Restoring muscular endurance is important after an injury. Your physical therapist with work with you to will develop a program of activities to help regain the endurance you had before the injury, and improve it.
Improve posture. Your physical therapist will teach you how to improve your posture so that pressure is reduced in the injured area, and healing can begin and progress as rapidly as possible.
Learn a home program. Your physical therapist will teach you strengthening, stretching, and pain reduction exercises to perform at home. These exercises will be specific for your needs; if you do them as prescribed by your physical therapist, you can speed your recovery.
Return to activities. We will discuss your activity levels with you and use them to set your work, sport, and home-life recovery goals. Your treatment program will help you reach your goals in the safest, fastest, and most effective way possible. For spine and leg pain from sciatica, your physical therapist may teach you correct ways to lift objects (called “body mechanics”) that will help protect your spine from aggravating symptoms.
Once your pain is under control or gone, it will be important for you to continue your new posture and movement habits to keep your back healthy and pain free.
To learn more about how physical therapists treat sciatica, listen to this informative episode of Move Forward Radio. In this episode, physical therapist and researcher Mark Bishop discusses the basics of sciatica. An expert on the condition, he also addresses how physical therapists treat the condition.
Surgery
In some cases, surgery is necessary to prevent further damage. If you undergo surgery for your sciatica, your physical therapist will work closely with you and your surgeon to help you regain motion and strength more quickly than you could on your own, and help you get back to your normal lifestyle as quickly as possible.
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat people who have low back and leg pain as a result of sciatica. You want to consider:
- A physical therapist who is experienced in treating people with orthopedic, or musculoskeletal, problems.
- A physical therapist who is a board-certified clinical specialist or who completed a residency or fellowship in orthopedic physical therapy. This therapist has advanced knowledge, experience, and skills that may apply to your condition.


 Ari is originally from Austin, TX. He received an undergraduate degree in Economics and Political Science from UC Santa Cruz, and a Master’s degree in Public Policy from University of Texas. After years of working in the public policy sector in Washington, DC and Austin, TX, Ari decided to make a professional change, return to school and received his Doctorate of Physical Therapy from Texas State University.
Ari is originally from Austin, TX. He received an undergraduate degree in Economics and Political Science from UC Santa Cruz, and a Master’s degree in Public Policy from University of Texas. After years of working in the public policy sector in Washington, DC and Austin, TX, Ari decided to make a professional change, return to school and received his Doctorate of Physical Therapy from Texas State University.